In summer, the song sings itself. ~William Carlos Williams
By: Jessica Cook MS, RD, LD/N (Director of Education)
Can’t stand the heat then get out of the kitchen! Although it isn’t summer quite yet it sure feels like it during the month of June in South Florida. Instead of spending your glorious summer days standing over the hot stove try utilizing fresh produce to create wonderful salads that require no cooking at all! Below are a few delicious fruits and vegetables that are in season in June. Get inspired by these ingredients and make a healthy, refreshing salad for a change! These are a few delicacies available in the spring and early summer:
- Honeydew Melon
- Beets
- Brussel Sprouts
- Green Beans
- Nectarines
- Pineapple
- Strawberries
- Snow Peas
So get in the kitchen and try some delicious spring produce after viewing this issue of Healthy Living with Diabetes!
Recipe: Brussel Sprouts & Baby Kale Salad
Servings: Serves 2
Ingredients
- 1 cup shredded Brussel sprouts
- 1 cup Baby Kale leaves
- ½ cup cherry tomatoes
- 1 tablespoon extra virgin olive oil
- 1 tablespoon fresh lemon fresh lemon juice
- 1 tsp. finely sliced chives
- 1/4 teaspoon freshly ground black pepper
- ¼ cup dry roasted unsalted almonds, chopped
- ¼ cup finely grated Parmesan cheese
Directions
Slice Brussel sprouts as thinly as possible using mandolin or food processor. In large bowl, whisk together olive oil, lemon juice, chives, salt and pepper. Add Brussels sprouts, tomatoes, baby kale, almonds and Parmesan cheese to large bowl with dressing. Toss until combined. Enjoy!
Questions & Answers that Shed Light on Blood Glucose Monitoring
By: William Kaye MD
Question 1. What blood sugar values should I strive for?
Answer 1: You should get your blood sugars as close to the “target range” without going “too low”
Question 2. Is the “target range” the same thing as the “normal range?”
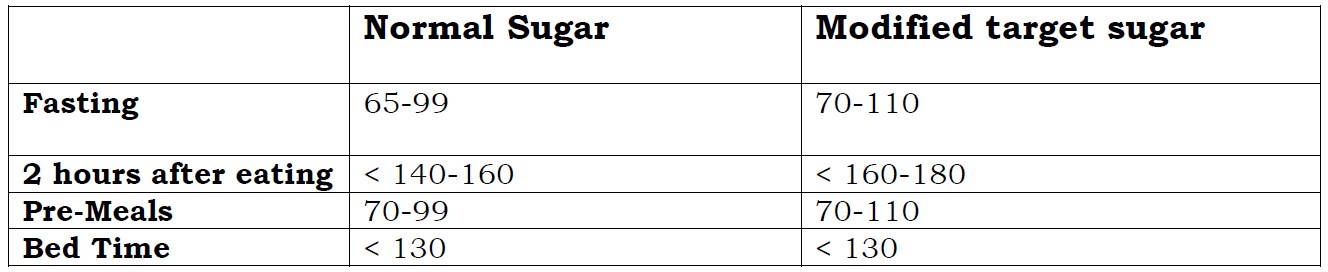
Answer 2: No! They are a little different. Below is a comparison. A “normal sugar” is the sugar that would occur in a healthy individual without diabetes and on no medications that could affect the sugar. A “target sugar” can be looked at as a modified sugar range. It is modified to still keep you free from the complications of high sugar, but also lesson the likelihood of a low sugar occurring. Below is a comparison of “normal sugars” vs. “target sugars”
Question 3. What is a low blood sugar?
Answer 3: Technically a low sugar is under 65, but there are different severities of “low sugars.” For all practical purposes there is mild, moderate, and severe low blood sugar. Let’s take severe first:
Severe hypoglycemia is when someone loses or almost loses consciousness from the low sugar or is so incapacitated they require assistance from someone else to come out of the low. Typically severe attacks occur when sugars go below 50, but the range is wide.
Moderate hypoglycemia is when someone experiences the typical symptoms of a low sugar such as difficulty concentrating, sweating, rapid heart rate etc., but can recognize and assist themselves to reverse the attack. Typically these types of attacks can occur between the sugar ranges of 50-65, but sensitive people can feel reactions at even higher sugars especially if their sugar is falling too fast.
Mild Hypoglycemia: Typically the individual has little or no symptoms and the sugar is marginally below normal i.e. less than 65.
Exceptions: The above three levels of hypoglycemia is a generalization. There are
some exceptions.
1. For example there are some people who can have a severely low blood
sugar for example “40” and feel perfectly normal. This is
called hypoglycemic unawareness or asymptomatic hypoglycemia.
2. Some individuals are can feel hypoglycemic despite normal values if
they have been running too high too long and normalization causes them
to feel the change or if their sugars fall too rapidly and they are measured
as they pass through the normal range on their way to hypoglycemia.
Question 4. If I get low sugars when I shoot for my target range despite everything I do, should my target range be changed?
Answer 4: If changing your medication, diet, and exercise regimen cannot avoid lows, then your doctor will set your target range higher to avoid these lows.
Question 5. If my morning sugars are normal, do I have to test other times?
Answer 5: Yes, because the pre-meal sugars are evaluating the affect of your last meal and the medications you take. For example pre-lunch sugars reflect the effect of your breakfast and medications (if any) on that value.
Question 6. If my sugars at a given time are always almost the same for example pre breakfast they are always 80-110 do I still have to test them daily?
Answer 6: No, if you are always getting the same value and you do not have plans to change your meals, medications, or exercise, and you are not going through a period of illness, stress or surgery, you can monitor the fasting sugars less often.
Question 7. What is the best way to manually log my sugars?
Answer 7: The best way to log sugars is to put the sugars in columns. Sugars done at the same time should be listed below each other. For example put breakfast under breakfast, pre-lunch under pre- lunch, pre- dinner under pre-dinner, bed under bed. This way you can easily follow patterns and trends and understand where your areas of excellence or areas of problems lie.
Question 8. Should I test 2 hours after meals?
Answer 8: Not everyone needs to test 2 hours after meals. If your fasting blood sugars, pre meal sugars, and bed sugars are within your target range but your HBA1c test shows the sugars are not good i.e. above “7,” then your doctor may look for what we call “hidden highs”. Hidden high sugars are sugars that you are experiencing, but not testing for. For example a patient may have a pre-breakfast sugar of 90 and a pre-lunch sugar of 100, but his 2 hour post breakfast sugar might be 230, which is too high. We look for hidden highs when the A1c is higher than what we expect by the other sugars. The other time when 2 hour testing is important is for pregnant patients with diabetes. These individuals need to test pre-meals and 2 hours after meals as normalizing their sugars is essential for the baby’s health.
Functional Health: New Me
By: Rosemarie Steinsapir MS, RD, LD, CDE
Years ago I saw health as physical or mental health. But what else would one associate with health? No one talked about functional health, as such. If I chose to improve my health by any small change, I pictured the outcome as having an impact on body systems and/or stress reduction.
Health, it seems, has a new suit of clothes which means different outfits for every person and maybe for everyday. This article is addressing Functional Health. (I happen to really like this focus on health because it can encompass everything from teeth to quality of life.)
Early in the 20th century, health focus was as much or more about living longer. Nutrition, vitamins and minerals took center stage and wow, did they perform! No one could imagine the developments that would come in this last century. Fleming opened the world to antibiotics, Salk to vaccines, and on and on. But as people lived longer and longer something began to happen in the 1970’s and 1980’s, we began hospice programs and the campaign for more quality of life began.
Functional Health refers to what your body can do now, and what you’d like it to be able to do in the future. It’s less about lab values and diagnostic numbers and more about standing up from a seated position, walking a mile and doing it pain free. This does not diminish or lessen the place for labs and health numbers, rather, to borrow from the camera man, it moves the perspective out to a more inclusive picture. It includes things such as sleeping deeply, eating joyfully, seeing life’s details (such as being able to thread a needle), or being able to twist in the driver’s seat to see the rear view window.
Some diagnostic values/numbers, such as cholesterol, may have a dramatic impact on functional health in the future. However, high cholesterol doesn’t feel any different than low cholesterol. The impact is in the future. Not so much with blood sugars. The everyday up and down for blood sugar is usually felt right away. It’s consequences for functional health is pretty dramatic too.
The message of functional health is to expand what we think of as a possible and expected outcome. Do you want to thread your own needle? – have the cataracts removed. Do you want to be able to do a mean tango when you’re seated next to the gorgeous cousin-of-the-bride? : Stretch the hip trochanter and quadriceps muscles and practice the steps to the tango now. Do you want to be able to quickly and sprightly get to the floor to welcome your grandchild’s first steps? : Get to the floor now and practice getting up and down.
Controlling both health numbers and setting a few functional goals (which are much more fun anyway), is a route to a life of quality.
Finally, for a really deep sleep, I recommend music. Music is fully and truly mind-bending, and tempo is the governing regulator. If you can make your own music, even better: piano, harmonica, etc. The tempo the human brain likes best is three quarter and four quarter time. Gregorian chant is known for releasing brain and central nervous system tension. And, so is dancing, with or without a partner!
At Healthy Living with Diabetes, we want to ensure that you are satisfied with all services received. We also would like your input on educational workshops that you would like us to offer, information you would like to read about in our Healthy Living with Diabetes Monthly or feedback on any workshop that you may have attended.
You can contact the director of education personally by email: jcook@PBDES.COM or leave a message at (561) 513-5100. We would love to hear from you!